
Fatigue: What Doctors Miss — Understanding the Thyroid–Adrenal Switch
Fatigue: What Doctors Miss — Understanding the Thyroid–Adrenal Switch
Waking up tired even after a full night of sleep, reaching for coffee multiple times a day, having gas and bloating, feeling emotionally fragile, and seeing lab tests that look "normal" — these are common complaints I hear every week. Many people get labeled with a thyroid problem, are started on medication, and then find their symptoms either do not completely resolve or return worse than before. The missing piece in many of these cases is what I call the thyroid–adrenal switch.
Why the thyroid and adrenals matter
Think of your body as having two main power engines: the thyroid and the adrenals. The thyroid sets your metabolic tone. It controls your basal temperature, metabolic rate, digestion, fertility mode, and overall energy production. When the thyroid is underactive, digestion slows, stomach acid decreases, and many downstream problems start. Gas, bloating, and recurrent gut infections such as H. pylori become much more likely because low stomach acid allows harmful bacteria to survive and flourish.
The adrenals are small but critical caps sitting above the kidneys. They behave like emergency generators. When you face stress, real or perceived, the adrenals produce cortisol, adrenaline, DHEA, and other hormones designed to mobilize energy fast. This is lifesaving in short bursts. But when stress becomes chronic, the adrenals can become overworked and dysregulated. That is when the thyroid and adrenals begin to interact in harmful ways.
What is the thyroid–adrenal switch?
In simple terms, the thyroid–adrenal switch happens when a sluggish thyroid forces the adrenals to take over metabolic responsibility. The body perceives this as an emergency. The brain signals the adrenals to produce emergency hormones so you can stay functional despite a slow thyroid. Initially you may feel an energy boost. That cortisol surge gives you a false lift, which makes it tempting to rely on stimulants like coffee.
When the stressor persists, the adrenals cannot keep up. Imagine running a generator on empty. Eventually, it sputters and you feel exhausted. At this point symptoms multiply: profound fatigue, poor sleep, anxiety, irritability, mood swings, and swings in blood sugar despite not being diabetic. This is not purely a thyroid problem anymore. It becomes an adrenal problem that feeds back to worsen thyroid function.
Why standard blood tests can miss the problem
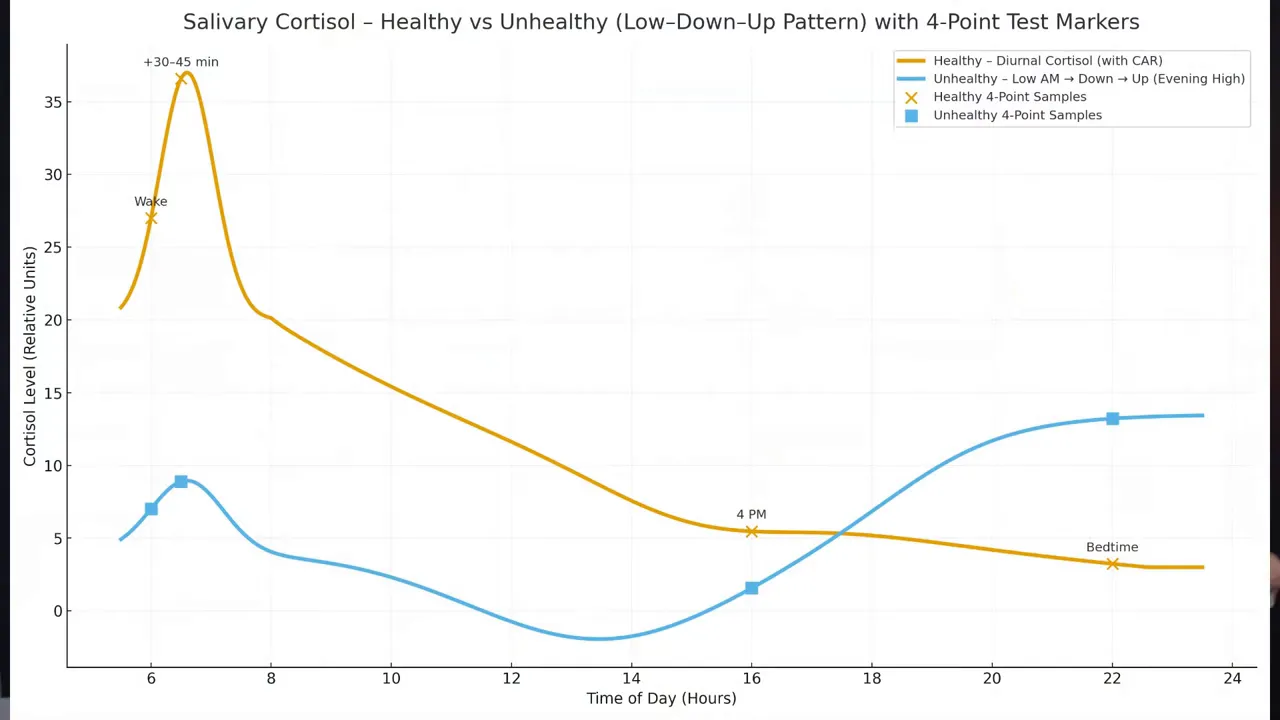
Most doctors measure cortisol with a single blood test, usually taken in the morning. That snapshot can be misleading because cortisol is not static. It follows a circadian rhythm with a peak in the morning and a gradual decline toward night. A single blood cortisol result can appear "normal" while the rhythm is completely off.
To see the true pattern, you need a 24-hour salivary cortisol profile taken at multiple points across the day. The typical protocol collects four saliva samples: early morning right after waking, mid-morning, evening, and late night. This produces a curve that shows whether cortisol peaks and declines in the expected way. In a healthy person the curve is high in the morning and steadily falls. In adrenal dysregulation the curve can be flattened, noisy, delayed, or even elevated at night.
What the salivary curve tells you
Healthy pattern: high morning cortisol with steady, predictable decline across the day.
High morning cortisol: may indicate acute stress or overactivation, often accompanied by poor sleep and anxiety.
Flattened curve: indicates adrenal exhaustion or blunted adrenal responsiveness.
Nighttime cortisol spikes: disrupt sleep and can cause waking at night without an apparent reason.
Erratic curve with multiple peaks: associated with mood instability, brain fog, and poor stress tolerance.
Unfortunately, salivary cortisol testing is not widely available everywhere and can be expensive in some countries. In India, for example, comprehensive testing and reverse T3 measures can cost a lot. When tests are unavailable or unaffordable, symptom-driven assessment becomes crucial.
How the adrenals affect blood sugar and thyroid hormones
Cortisol raises blood sugar rapidly by stimulating glucose release from the liver, breaking down muscle protein, and promoting gluconeogenesis. That rapid glucose increase can be followed by a crash. People caught in this cycle experience bursts of energy then sudden fatigue. They may mistake these swings for normal variation or attribute them to sugar or caffeine intake, but the underlying driver is cortisol dysregulation.
High cortisol also interferes with thyroid hormone metabolism. The body produces T4, which must be converted to the active form T3 to be usable. Chronic high cortisol impairs the T4 to T3 conversion and favours production of reverse T3, an inactive form that blocks thyroid receptors. This biochemical change makes the thyroid functionally worse even when standard thyroid labs like TSH or total T4 appear normal.
Reverse T3: another common blind spot
Reverse T3 testing can reveal what is happening at the tissue level, but it is costly and often not ordered. In many places, the reverse T3 test is expensive and difficult to access. Because of that, many patients who report hypothyroid symptoms and have “normal” TSH are told nothing is wrong. Yet if reverse T3 is high, it indicates that T4 is being converted into an inactive form under stress, which explains persistent symptoms.
When reverse T3 is elevated, it is a sign that the body is in a protective or stressed state. The body essentially slows metabolic processes to conserve resources. This is adaptive in short-term crises but harmful when persistent.
Common mistakes that flip the switch
There are several lifestyle and health patterns that push the thyroid–adrenal switch. Here are the most common:
Disrupted circadian rhythm: staying up late, inconsistent sleep schedules, and immediate morning screen exposure (blue light) prevents proper morning cortisol production and disturbs the rhythm.
Unsupervised or extreme fasting: prolonged fasting, repeated skipping of meals, and extreme protocols like frequent 72-hour fasts can trigger stress responses when the body is already nutritionally deficient. Autophagy is a real process, but it is not a goal to pursue on an undernourished or mineral-deficient body.
Chronic gut infections and inflammation: H. pylori, small intestinal bacterial overgrowth, and candida can create chronic inflammatory stress in the body, keeping cortisol elevated and the adrenals engaged.
Toxins: environmental toxins, mold and mycotoxins, and contaminated food create ongoing physiologic stress. These can cause unexplained anxiety and fatigue even when your life is not objectively stressful.
Micronutrient deficiencies: low vitamin D, magnesium, zinc, iron, and other deficiencies lower resilience. Even mild deficiencies magnify stress responses and prevent recovery.
Symptoms that suggest adrenal involvement
When the adrenals are part of the problem, symptoms extend beyond classic hypothyroid complaints. Look for:
Severe or unusual fatigue that does not improve with thyroid medication alone
Waking at night for hours, unable to fall back to sleep
Anxiety, irritability, mood lability, and increased sensitivities
Blood sugar swings without diabetes
Dependency on stimulants such as coffee or energy drinks
Salt cravings or lightheadedness when standing
What to do: a practical recovery plan
Recovering from a thyroid–adrenal loop requires a multimodal approach that addresses sleep, nutrition, stress physiology, gut health, toxins, and micronutrients. Here is a practical plan you can start implementing today.
1. Restore circadian rhythm
Go to bed and wake up at consistent times every day. Aim for wake-up time aligned with sunrise if possible.
Avoid screens and bright blue light for at least 30 to 60 minutes after waking and 60 to 90 minutes before sleep.
Get at least 10 minutes of morning sunlight exposure. This helps trigger the proper morning cortisol peak and sets your circadian clock.
2. Prioritize nutrient-dense, balanced meals
Adrenal support requires adequate salt and healthy fats. Do not be afraid of salt if you have normal blood pressure and no contraindications. The adrenals need sodium to produce hormones and maintain blood pressure. Avoid extreme low-fat or ultra-low-salt diets when recovering from adrenal fatigue.
Ensure each meal has a balance of protein, fat, and carbohydrates.
Include good quality proteins like eggs, fish, poultry, red meat, or paneer for vegetarians.
Include healthy fats: olive oil, ghee, coconut oil, avocado, and nuts.
Address deficiencies with targeted supplements when necessary after testing or under guidance.
3. Use an adrenal cocktail wisely
When you need a quick, gentle lift that supports adrenal physiology, a simple "adrenal cocktail" can help. Mix water with a pinch of real, mineral-rich salt (pink salt or unrefined salt) and fresh lemon juice. This provides sodium, trace minerals, and a little vitamin C. The adrenals appreciate both salt and fat, so pairing this with a protein- and fat-containing breakfast is ideal.
4. Reduce stimulant dependence
Caffeine and many "energy" products act as stimulants and can mask underlying dysfunction while worsening adrenal load. If you rely on multiple coffees to get through the day, consider slowly tapering rather than quitting abruptly. Replace some coffee with morning sunlight exposure and the adrenal cocktail for more sustainable energy.
5. Improve sleep quality
Create a wind-down routine: dim lights, limit heavy meals before bed, and do relaxing activities.
Address nighttime cortisol spikes by evaluating stress, sleep environment, and possible toxin exposures. If you wake at night and cannot return to sleep, consider gentle breathing techniques and reducing stimulants late in the day.
6. Learn box breathing to calm the system
Box breathing is simple and can be done anywhere. It strengthens the gut-brain connection and signals safety to your nervous system.
Inhale gently for a count of four.
Hold for four.
Exhale for four.
Hold for four.
Repeat for 3 to 5 minutes or until you feel calmer.
7. Investigate gut infections and inflammation
Persistent gut problems like H. pylori or candida can create chronic physiologic stress. Low stomach acid from hypothyroidism makes these infections more likely. Treating gut infections without addressing underlying thyroid and adrenal dysfunction often leads to recurrence. Evaluate digestion, stool patterns, and consider professional testing and treatment when indicated.
8. Look for toxins and mycotoxin exposure
Toxins, mold, and mycotoxins are stealth stressors. They can cause fatigue, brain fog, and mood problems without any obvious external stressors. If your environment is damp or you suspect mold exposure, address it quickly. Detoxification is a long, sometimes costly process, so prevention and mitigation are worth prioritizing.
9. Correct micronutrient deficiencies
Vitamin D, magnesium, zinc, iron, B12, and other micronutrients are essential for energy production and stress resilience. Even mild deficiencies can keep the body in a stressed state. Test and correct these deficiencies with food-first approaches and supplements when needed.
How to approach testing when resources are limited
When salivary cortisol and reverse T3 testing are not available or affordable, decisions should be based on symptoms, patterns, and careful clinical reasoning. I have built tools that help interpret symptoms to identify likely system breakdowns, but you can start by tracking:
Sleep and wake times and how rested you feel each morning.
Daytime energy patterns and when crashes occur.
Caffeine use and how it affects your mood and sleep.
Cravings for salt or sugar and post-meal symptoms.
Gut symptoms and any known infections or antibiotic history.
These simple records often reveal patterns consistent with adrenal involvement even when standard blood tests look normal.
When to seek professional help
If you experience severe fatigue, frequent syncope, dramatic drops in blood pressure, severe mood disturbances, or any alarming symptoms, seek medical attention promptly. For chronic, non-urgent symptoms that suggest a thyroid–adrenal loop, look for a practitioner who understands functional medicine, circadian endocrinology, and the interaction between thyroid and adrenals.
Be cautious with medication adjustments. Thyroid hormone replacement can help, but if the adrenals are supporting thyroid function under stress, simply increasing thyroid medication without addressing adrenal health may worsen symptoms or create dependency on stimulants.
Realistic timeline and expectations
Recovery from adrenal dysregulation and a thyroid–adrenal switch is not overnight. It often takes months to rebalance sleep, nutrition, toxin load, and micronutrients. Expect gradual improvements if you consistently address the root causes: better sleep, less stimulant dependence, balanced meals, toxin mitigation, and targeted support for deficiencies and gut health.
Measure progress by changes in energy stability, sleep continuity, mood resilience, fewer cravings, and improved digestion. If available, repeat salivary cortisol profiles and thyroid function tests, including reverse T3, to track biochemical improvements over time.
Practical daily checklist to prevent the switch
Wake up at a consistent time and get 10 minutes of sunlight soon after waking.
Avoid screens first thing in the morning and an hour before bed.
Eat regular, nutrient-rich meals with protein, healthy fat, and complex carbs.
Include a pinch of mineral salt and fresh lemon in water if you feel low in the morning.
Practice box breathing for 3 to 5 minutes daily, especially during moments of stress.
Address any gut symptoms with a healthcare professional and test if needed.
Check and correct common micronutrient deficiencies.
Limit and slowly taper stimulants rather than abrupt quitting if you depend on them heavily.
Final thoughts
Fatigue is rarely caused by one isolated issue. The interaction between thyroid and adrenal function is a powerful and often overlooked contributor to persistent fatigue, mood disorders, sleep disturbances, digestive problems, and blood sugar swings. You can feel better by addressing the whole system rather than chasing a single lab value.
Start with sleep and circadian restoration, prioritize nutrient-dense meals with adequate salt and fat, reduce reliance on stimulants, practice simple breathing techniques, and investigate gut and toxin-related causes when symptoms point that way. Where possible, use a 24-hour salivary cortisol profile and consider reverse T3 testing to uncover hidden dysfunctions, but do not let lack of testing stop you from making practical, symptom-driven changes today.
If you track your symptoms, make small consistent changes, and focus on rebuilding resilience rather than quick fixes, your energy, mood, and digestion will likely show steady improvement.
